The
loss of an eye through accident, disease or from congenital disorders is a
significant life event that impacts on a person's self-image, confidence and
wellbeing. It warrants on the part of the affected person to undergo perceptual
adjustments because of the loss of binocular cues to depth and the reduction in
visual field on the affected side. While the prosthetic eye comes as a boon for
cosmetic rehabilitation, the person also would have to make a behavioral
adaptation because they need time and training for wearing and maintaining the
prosthesis.
A
prosthetic eye is designed to restore the appearance of the eyeball and partly
the function of the eyelids. The term 'ocular prosthesis' is used throughout
this writing, however, other terms like 'prosthetic eye' and 'artificial eye'
can also be used synonymously.
The
absence of ocular tissue in the orbit is considered as anophthalmia, which can
be both congenital and surgical. The anophthalmic eye socket resulting from
enucleation after trauma, painful blind eye, endophthalmitis, intraocular
malignancy or phthisis bulbi due to various causes may lead to several social,
familial and psychiatric problems. After surgically removing the eyeball, an
artificial eye is placed instead in order to improve the aesthetic values of the
disfigured face. Therefore, ocular prosthesis is a form of prosthetic device
that is positioned in orbit with or without replacement of ocular tissues to
alleviate the cosmetic appearance of the face. A disease and its treatment do
have their own inherent qualities that bring about a range of consequences
including changes in psychosocial behavior.
World History of Ocular Prosthesis
We
have seen vintage old-movies scenes where pirates patch one eye to obscure facial
disfigurement as a result of unilateral eye loss. Due to physical threats, wild
animal encounters and war, losing one eye and accepting it with just a fabric
or leather patch had become a lifestyle. The first report of ocular prosthesis,
however, dates back to 2900-2800 BC in Iran and was presumably made up of gold
plated bitumen paste with central iris engravings, with a diameter around 2.5
cm (Sajjadi, 2007) Egyptians and
Roman priests made prosthesis by painting the clay which the Greek termed
Ekblebharon (worn in front of the eyelid)(Chalian VA, Drane JB, 1971).
Ambrose Pare, a
Frenchman, is believed to be the first person who devised an in-socket
prosthetic eye in the sixteenth century (E, 1968). Pare was also
assumed to be the person to design hypoblepharae (prosthetics worn inside the
eyelid)(Chalian VA, Drane JB, 1971). During those
times, prosthetic eyes were primarily made up of metals, woods, ivory and
glass. For a brief period of the 1700s, Paris became the hub for manufacturing
prosthetic eyes where Auguste Boissenneu made thin enamel shells on order which
could be worn over shrunken eyes. A German doctor Friedrich Phillip Ritterich
did not like the overpricing of the prosthetics in Paris and hence started to
make cheaper ones in Germany though the crude materials had to be brought from
Paris. He encouraged German glassblowing industries to make artificial eyes and
established free eye glass service at his Leipzig Eye Institute.
The
quick adaptation of technology by the Germans made Germany a new hub for
prosthetic makers in the mid 19th century (Smith BC, Della Rocca RC). The year 1880
saw 'reform eyes' − a hollow glass eye with round edges, developed by Dutch
ophthalmologist Hermann Snellen. Germany became the largest exporter of stock
eyeglasses made from Cryolite glasses in the 1900s. The field of ocular
prosthesis revolutionized later in 1930s after the introduction of PMMA
materials by Imperial Chemical Industries (ICI) under various market names:
Plexiglas, Lucite, Perspex, etc.(Kollewe J). At this time
the prosthetic eye was clearly falling under the practice scope of dental
technicians because molding and curing was quite similar to that of vulcanite
rubber essential for dentures. Fritz W. Jardon, a German dental technician who
migrated to USA and joined American Optical Company in 1930s; this made a clear
way to successfully adopt mass production of high-finished PMMA prosthetics
with worldwide supply capacity. Lately, silicone prosthetics have arrived in
the market but has not replaced PMMA yet.
As
has been discussed, dental technicians felt the need that since making ocular
prosthesis was under their professional arena, they should be further expanding
and strengthening their expertise in this particular subject. This led to the
formation of a new discipline called maxillofacial prosthetics, that enabled
the dental professionals to legally and openly address the people by ocular
prosthetic rehabilitation. At some point, role of optometrists seemed to be
caring eyes only until they stopped to see. The Americans reformulated the
concept to encompass the ocular prosthetic division under 'ocularistry', a
branch of ophthalmology, while the English ideology focused on dental
technology until later. American Society of Ocularists (ASO) was established in
1957; they standardized the profession of ocularist with requirements of
training and certificatio (N., 2006). Manufacturing
process had now embraced many avant-garde approaches like computer aided
designs, CNC technologies, photographic adaptations, etc.
Scenario of Ocular Prosthesis in Nepal
Similar
to world history, the ocular prosthesis were, for a long time, made by dental
professionals and these skill sets are largely claimed by maxillofacial
prosthodontists. Major bulk of making ocular prosthesis is still in those
hands. People's Dental College is the oldest dental college of Nepal and its
faculty members have been involved in not only making but also in ocular
prosthetic rehabilitative services. In the 2000s, many eye hospitals of Nepal
started to offer stock fitting prosthetic eyes. They are available to public
purchase from a few hundred to fifteen hundred Nepalese rupees. It was only in
January 2012 AD that an Ocularist unit was established in an eye hospital for
providing prosthetic services in Nepal (Adhikary R and Shrestha K, 2020) The pioneering
endeavor was undertaken by Tilganga Institute of ophthalmology (TIO). Since
then the unit is manned by a senior ophthalmic assistant Mr Kumar Shrestha, who
was trained on ocular prosthetic procedures and fitting techniques. Eye health
worker Sabita Chamling Rai also helps him in the unit as an adjunct. The unit
has made and fitted over one thousand customized prosthetic eyes. Since TIO's
ocular Oncology and oculoplastic department is nation's referring point for
many ocular carcinomas and ocular disfigurement, it serves as the good feeder
for the cases to the ocularist unit.
After
about six years, Dhristi Eye Care System has also started its daily ocularist
unit at Kalanki and occasionally (monthly or bimonthly) in Jhapa. The unit was
first manned by optometrist Ravi Shankar Chaudhary, but has now recently left.
Few other private clinics also offer prosthetic services in major cities of
Nepal. Though the global ocular prosthesis has already witnessed state-of-the-art
technologies in its design and fabrication, Nepal is still relying on manual or
semi-manual techniques.
Anophthalmia
The
absence of ocular tissue in the orbit is considered as anophthalmia. Congenital
form of anophthalmia can be categorized into true anophthalmos where there is
complete absence of ocular tissues and clinical anophthalmos where there are
evidences of neuro-ectodermal tissues in histological sectioning (Verma and FitzPatrick, 2007). Since extreme microphthalmia also
requires prosthetic rehabilitation, and is intermediary between anophthalmos
and microphthalmos, we tend to keep it under the category of anophthalmia.
Anophthalmia can also be an acquired condition due to trauma, phthisis bulbi,
atrophic bulbi, contracted socket, staphyloma and surgical procedures like
enucleation, evisceration and orbital exenteration (Raizada and Rani, 2007). Ocular prosthesis is a form of prosthetic
device that is positioned in the orbit with or without replacement of ocular
tissues to alleviate the cosmetic appearance of the face.
The Anophthalmic Socket
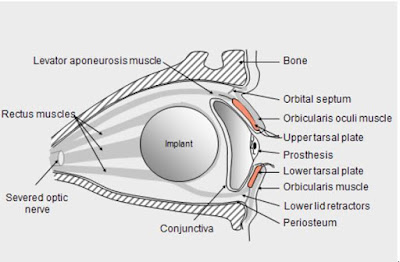 |
| Figure 1: The Anatomy of anophthalmic socket |
The
successful fitting of ocular prosthesis largely depends upon the status of
anophthalmic socket, which is where the artificial eye rests upon the
biological structures of the orbit. The integrity of the socket might also be
disrupted due to unnatural physical insults or trauma. Above figure clearly
outlines the structural environment of a normally expected anophthalmic socket
with an implant in situ.
Types of Eye Removal Surgeries
Eye
removal is mandated in certain circumstances like retinoblastoma, painful blind
eye, trauma to mitigate sympathetic ophthalmitis, etc. It is also done in the
black fungus infection, an uncommonly encountered post-COVID manifestation, to
stop the spread of infection beyond orbit and hence to save life. Surgical
removal of eyeball consists of three approaches:
a) Enucleation
The
surgical technique that removes just the eyeball or globe leaving the
conjunctiva, tenon's capsule, extraocular muscles and the stub of optic nerve
in their own place is called enucleation. This is the most common eye removal
surgery and is assumed to be also the oldest operation in the field of
ophthalmology (Moshfegi, 2000). By the
prosthetist's point of view, enucleation is superior in that they offer ample
space for larger implants, and furnishes better cosmesis. It also has lesser
risks for sympathetic ophthalmitis when compared to evisceration (P, Viswanathan; Mandeep S, Sagoo; Jane M, no date). Intraocular
tumors, including retinoblastoma and uveal melanomas, have been the primary
indication for enucleation.
b) Evisceration
The surgical procedure is called evisceration when only the viscera or intra-ocular contents of the eyeball is removed. That means uvea, retina, vitreous, lens are removed so that sclera will be left. The technique is simpler and less invasive than enucleation and it provides better motility of the ocular prosthesis and ensures stability of the anophthalmic socket (Chen, 2001). The major indications of evisceration have been painful blind dye due to endophthalmitis, corneal perforation and secondary glaucoma.
c) Orbital Exenteration
This is more of an extrusive surgical technique whereby all the intra-orbital contents, typically including the conjunctiva, globe, orbital fat, part or all of the lids and sometimes a portion of the bony orbit are removed leaving patients severely cosmetically disfigured. The esthetic rehabilitation cannot be fulfilled by ocular prosthesis alone. It warrants maxillofacial prosthesis. Hence, this most radical of procedures is reserved for patients with large, highly invasive orbital tumors which may have originated from within the orbit or from the surrounding orbital structures.
Implants and Conformers
The
average volume of the eyeball is 6-7 ml and once the eyeball is removed, the
volume should be substituted with intra-orbital implant and prosthesis. The
characteristics of an ideal implant should be: 1) it should provide ample space
to the fitting and motility of prosthesis 2) it should be stable enough to
restore the intra-orbital integrity 3) there should be no risk of extrusion.
Implants
are of two types according to the nature of their connection to the adjacent
ocular tissues. Non-integrated orbital implants are mostly spherical and made
up of PMMA or silicone material and are not directly attached to the extraocular
muscles, whereas bio-integrated orbital implants are the ones that have
connection points, holes or channels to facilitate the attachment of extraocular
muscles. The connection renders a sort of ocular motility while in different
gazes. Earlier forms of integrated implants were Iowa implants and Allen
implants but now these are largely replaced by hydroxyapatite coral implants
with porous surface that allows fibrovascular sheathing for better attachment.
The central drill also would make a hole where a peg can be inserted whereby
the peg constitutes the bridging component between implant and outer cosmetic
prosthesis. This enabled increased ocular motility but, unfortunately, it was
not without complications and obviously it needed extra surgical effort for
drilling and putting up the peg. Other common integrated implants used in
today's practice are porous polyethylene, aluminium oxide and bio-ceramic among
others. In case the implant is not porous, it
is wrapped with donor sclera, preserved bovine pericardium, human fascia lata or vicryl mesh in order to
impart the biocompatibility.
Post-surgical
conformers are put outside the conjunctival surface after an implant is
inserted and sutured from the outside. The eye is then pressure-patched for
24-48 hours. These conformers are made up of silicone or clear PMMA materials.
The aim of putting conformers are: 1) it preserves the fornices intact 2) it
protects the conjunctival wound underneath and accelerates healing process
thereby avoiding implant extrusion 3) it makes the space ample for future
prosthetic fitting. Since conjunctival healing may bring about some form of
contracture, there should be no delay in putting the new prosthesis before
complications, like discharges, inflammation and socket contracture take place.
Generally, a month of gap between enucleation surgery and prosthetic placement
is expected.
Figure 2: Post-surgical conformer Right Eye
Eye Loss
Unilateral
eye loss brings about having to change the ways you interact with the
environment. This is because having only one eye functioning means your visual
world shifts to the side of your seeing eye. Over the long run, perceptual
adaptations virtually neglect the side of your non-seeing eye. So, you have to
adjust your head i.e. turning the face towards the defective eye is a common
occurrence because visual system tries to compensate the reduced visual field
offered by a single eye. This may sometimes afflict people while trying to
cross the busy road or driving.
Monocular
vision also means that you have lost the cues for binocular depth perceptions.
This limits a person from performing fine activities that demand sharp stereo-acuity,
like needling. They are also deprived from enjoying 3D movies in theatres while
their friends enjoy normal life unbeknownst to the fact that one of their
friends cold not see what they could.
Psychosocial Aspect and Quality of
Life (QoL)
Losing
an eye has a far-reaching impact on a person's life especially on how s/he
feels about herself/himself and this will alter how s/he interacts with other
people. A disease and its treatment do have their own inherent qualities that
bring about a range of consequences including changes in psychosocial behavior (Zboralski et
al., 2008). World Health Organization has
defined a health as a state of complete physical, mental and social well-being
and not merely the absence of disease or infirmity (Kelley, 2008). This widely
talked about ‘well-being’ is linked with quality of life (QOL), which is now a
global concept that encompasses mental, social and physical activities that
could be affected negatively by disease and infirmity or positively by good
physical and mental conditions (Zboralski et
al., 2008). Since quality of life (QOL)
carries a broader meaning, health related quality of life (HR QOL) has been
used in health researches to represent QOL particularly affected by a health
condition. So, this perceived well being gets affected once an eye is lost.
Many studies have tried to quantify the quality of life with scores in order to
easily analyze, compare and interpret them.
Eye
loss is an event in life that does not only entail the physically absent eye.
It does have a lot of psychosocial consequences as well. We can even
arbitrarily check this status of anophthalmic patients by administering a quick
Hospital Anxiety and Depression Score (HADS) questionnaire. Many people,
particularly adolescents, fear the negative body image due to eye loss. This
may, at times, severely limit their social activities, participation and
overall development.
As
we come to know that the absence of orbital content makes the surrounding
tissues hypo-functional and may become atrophied, individually fabricated
prosthetic eye not only plays an important role in the functional restoration
partially but also cosmetic enhancement in the appearance (Goiato, de Caxias and dos Santos, 2018).
Corneal Tattooing, Prosthetic
Shell, and Prosthetic Eye
Corneal
tattooing is a less invasive procedure which involves making micro-punctures on
the scarred cornea and putting the shades of drawing ink in the anterior stroma
to give matching color to the fellow eye. If the eye is of similar size then
tattooing will fulfill the demand of cosmesis. However, if the size is smaller
we have to go for a prosthetic shell or prosthetic eye. Corneal tattooing has a
dual purpose: 1) esthetic: if the patient can't wear cosmetic contact lens the
corneal scar should be painted black or blue with the tattoo 2) functional: the
seeing eye can be sometimes photo-sensitive due to partial/complete aniridia or
albinism where pupillary zone is peripherally blocked by the tattoo.
Figure 3: Corneal tattoo
Prosthetic
shell is a thin prosthetic device that fits over a phthisical eye. The central
thickness of such a shell is less than 1 mm. If the globe is still remaining
but with small size and whitish cornea, then prosthetic shell might be a good
indication since it widens the palpebral aperture by lifting the upper eyelid
and obscures the corneal opacity.
Ocular
prosthesis or simply prosthetic eye is a prosthetic device that helps to
restore the orbital integrity in the absence of an eyeball. Ideal prosthesis
not only fills the orbital area but also maintains the lid tonus and
facilitates the circulation of tears. Indeed, ocular prosthesis is not
recommended and used only for cosmesis, it has numerous functional and anatomic
importance as well. It prevents the deformation of eyelids; it also imparts the
fullness to the anophthalmic cavity preventing muscle atrophy. It constantly
facilitates the right and healthy orientation of lacrimal flux and checks
debris accretion. It is for this reason that the anophthalmic children be
fitted with the prosthesis so that the facial symmetry is preserved for long as
it allows normal growth and development of hard and soft tissues of the
surrounding.
Procedures for Customized Ocular
Prosthesis Fabrication
Generally
fabrication of a customized ocular prosthesis consists of the following steps:
a) Impression:
a plastic impression tray is placed in the anophthalmic socket where impression
materials (mostly alginate powder) are injected through the central pipe after
mixing in the water in approximately 1:1 ratio from the nozzle of a syringe.
Alginate is an elastic, irreversible hydrocolloid impression material which
quickly sets (in about less than a minute) to the contours of ocular surfaces
beneath the eyelids. The impression is then taken out.
Figure 4: Re-usable impression trays
b) Wax conformer:
The impression is put in a plastic cup and is poured over by alginate powder
mixed with water as above. After it sets out, we can take out the impression by
dissecting the elastic alginate. The void formed in the alginate material is
then filled by pouring melted wax. After some time, the wax conforms to the
interior contours of the alginate mold. The wax sphere has the matching
contours with the ocular surfaces. Errors of impression can be corrected in
this step and many adjustments can be done through wax conformers like ptosis,
lid sagging, excessive gaps, etc.
Figure 5: Making wax conformer
c) Centration
: After cooling, the wax sphere is separated out and further smoothened. It is
inserted into the patient's socket and watched for the appropriate fit and
centration of the pupil by a marker, with the patient in the standing position
looking straight ahead and in a good lighting condition. The marker would signify
the point where the iris button of closely matching color is centralized.
Figure 6: Iris
d) Two-part mold:
The wax model creates an impression in the plaster of Paris (stone mould) put
in the two-part metal mold. The hollow spherical zone is now filled with
acrylic (methyl methacrylate powder) material and is put for polymerization
either in the polymerizer or in the heating pressure cooker. In a few hours,
white PMMA prosthesis is made with an iris.
Figure 7: two-part molds
e) Hand painting:
PMMA prosthesis is inserted into the eye and looked for color discrepancies in
natural light. Then color tainting is done with a hand brush with the addition
of blood vessels with tiny red threads to give a more natural look. In some
setting, the replica of iris is produced by digital imaging of the fellow eye.
Figure 8: Hand painting to match the
color
f) Final layering with clear PMMA
: The final stage consists of overlaying of clear PMMA through a process of
polymerization over the semi-finished white PMMA prosthesis. It is done for a lustrous
look and for a 3D appearance so as to give an illusion of virtual AC
depth.
Figure 9: before undergoing clear PMMA
polymerization
Stock Prosthesis vs Custom made
prosthesis
Stock
prosthesis are the ready-to-use prosthesis manufactured in mass quantity with
the general parameters, color and sizes. They are relatively cheap as
production is made in large scale. But, it may not exactly match the iris
color, size and shape of the fellow eye. It cannot be modified per the need of
patients and the life span of stock prosthesis is generally 1-2 years. Since
the fitting is not as par, there are obvious reasons why these prosthesis are
full of post-fitting complications like inflammations, deposits, allergies,
excessive discharges and non-tolerances.
Custom
made prosthesis (CMP) is person-specific and it exactly matches the contours of
ocular surface. Hence it allows for minimal movement to give a somewhat natural
look unlike stock prosthesis. Complications are also minimal owing to the close
alignment of the prosthesis to the underlying surface. If there is no void,
there are less chances of accumulation of tears and debris that might form
colonizing zones for infectious organisms. The durability of CMPS is about 7-10
years according to the handling behavior of the patients. It can be polished,
resurfaced and adjusted as per needed.
Common Complications associated
with the wearing of ocular prosthesis
The
common complications encountered by the patients while wearing a prosthetic eye
can be shortly summarized as below:
(a) Discharge
Discharge
is probably the most common ocular problem faced by the prosthetic wearers.
While it is less pronounced in comparison to those wearing stock prosthesis,
the problem appears to rise as the prosthesis ages. The problem of discharge
arises due to two factors: one; mechanical irritation and two; infection.
White, ropy discharge is an indication of allergy due to the mechanical
friction against the ocular surfaces. We can observe the giant papillary
reactions at the palpebral conjunctiva, more conspicuously in the upper
palpebra. A combination of corticosteroid (prednisolone or dexamethasone) with
longer dose of sodium cromoglycate is the standard mode of treatment with the
regimens depending upon the severity. Yellow muco-purulent discharge is, on the
other hand, an indication of bacterial infection.
(b) Discomfort
Another commonly seen problem with the prosthetic wearers is the ocular discomfort with the wear. The discomfort generally arises from two factors: either there is a problem in the prosthetic eye itself like scratches, rough deposits, chips broken out, sharp edges, faded coats, etc., or there is problem in the ocular surfaces like new malignancies, socket contracture, infections or extrusion of implants. Therefore, the prosthesis should be taken out and scrutinized quite carefully to see any abnormal surface and deposit. If there is any, then it should be buffed out by polishing. If the problem is associated with the ocular surface, it should be treated accordingly which may sometimes even warrant surgeries, for example, in the case of implant exposure, contracted socket syndrome or malignancy.
(c) Dry Eye
Since
the ocular surface is highly compromised in anophthalmos and it is even more
when there is a prosthetic eye constantly kept in the socket as a foreign body.
Hence, the tear volume is less than expected and due to less and compromised
goblet cells the quality of tear is also poor. The frictional force against the
lid may sometimes give rise to scars and fibrosis along the conjunctival lining.
These all result in nothing but a dry eye. The dry eye can be treated by
applying lubricating viscous drops like HPMC and CMC. More severe form may
mandate 100% medical grade silicone oil which lasts for a relatively long time.
Corticosteroid and Cyclosporine A are other options in severe dry eye but these
drugs should be used cautiously.
(d) Lid sequelae
The
prolonged uses of prosthetic eye may sometimes result in lid sequelae like lid
laxity and ptosis. Ptosis is commonly corrected by adjusting the prosthesis
whereby PMMA material is added to lift the superior part of the prosthesis so
that it pushes the levator palbepral superioris muscle and abates the degree of
visible ptosis. If this type of prosthetic adjustments are done many a time,
then consultation with the OPAL surgeon should be made to explore the surgical
options for making good ocular spaces. Similarly, contracted socket also
requires renovation of the orbital surface to increase the volume for the
comfortable prosthetic insertion and acceptable movement.
(e) Implant related complications
Sometimes the implant might be exposed causing pain. The problems with the implant are magnified if there is a pegged implant. For example, the peg can be broken or its surrounding may harbor bacterial colonies increasing the risk of infections. The patient with these problems should be recommended to visit an OPAL surgeon for a surgical correction.
1.1.13 Three-D printed Ocular
prosthesis
Esthetically
appealing and functionally superior ocular prosthesis can be made in modern
days by the 3-D printing technology which mainly utilizes Computer Aided
Designing (CAD) and Computer Aided Manufacturing (CAM). The process is
generally also called as Bio-CAD modeling and is just not used in ophthalmology
but also in dentistry and orthopedics (Alam et al.,
2017).
The model developed from the medical image processing is adapted to CAD
to finally 3D print through rapid manufacturing machine or Polyjet 3D printer.
The material used in this process is, as above, medical grade biocompatible
Poly Methyl Metha -Acryate (PMMA).
References:
Adhikary R, Shrestha K. (2020) ‘Artificial eye: Boon
for those with no eyeball’, The Himalayan Times, 5 March. Available at:
https://thehimalayantimes.com/opinion/artificial-eye-boon-for-those-with-no-eyeball
Alam, M. S. et al. (2017) ‘An innovative method of
ocular prosthesis fabrication by bio-CAD and rapid 3-D printing technology: A
pilot study’, Orbit, 36(4), pp. 223–227. doi:
10.1080/01676830.2017.1287741.
Chalian VA, Drane JB, S. S. (1971) Maxillofacial
prosthetics: Multidisciplinary practice. Baltimore: The Williams and
Wilkins Co.
Chen, W. P. (2001) Oculoplastic Surgery: The Essentials.
New York: Stuttgart: Thieme. doi: 10.1055/b-002-41864.
E, W. (1968) Anatomy of the eye and orbit. 6th ed.
London: H K Lewis & Co. Ltd.
Goiato, M. C., de Caxias, F. P. and dos Santos, D. M. (2018)
‘Quality of life living with ocular prosthesis’, Expert Review of
Ophthalmology, 13(4), pp. 171–173. doi: 10.1080/17469899.2018.1503534.
Kelley, L. (2008) ‘The World Health Organization (WHO)’, The
World Health Organization (WHO), (October), pp. 1–157. doi:
10.4324/9780203029732.
Kollewe J, W. G. (no date) ‘ICI: from Perspex to paints’, The
Guardian. Available at: www. guardian.co.uk.
Moshfegi, D. M. A. (2000) ‘Enucleation’, Surv Ophthalmol,
44, pp. 270–301.
N., H. (2006) Artificial eyes and the artificialisation of
the human face. C Timmerma. Basingstoke: Palgrave.
Le Grand Associates. Available at:
http://www.legrandeyes.net. (Accessed: 9 October 2021).
P, Viswanathan; Mandeep S, Sagoo; Jane M, O. (2006) ‘UK
national survey of enucleation, evisceration and orbital implant trends’, Br
J Ophthalmol., 91(5), pp. 616–619. doi: 10.1136/bjo.2006.103937.
Raizada, K. and Rani, D. (2007) ‘Ocular prosthesis’, Contact
Lens and Anterior Eye. doi: 10.1016/j.clae.2007.01.002.
Sajjadi, M. (2007) ‘5,000-year-old artificial eyeball found
in Iran’, Times of London, 21 February. Available at:
https://historynewsnetwork.org/article/35645.
Smith BC, Della Rocca RC, N. F. (2012) Ophthalmic plastic
and reconstructive surgery. Edited by V. III. St. Louis: C.V. Mosby Co.
Verma, A. S. and FitzPatrick, D. R. (2007) ‘Anophthalmia and
microphthalmia’, Orphanet Journal of Rare Diseases, 2(1), pp. 1–8. doi:
10.1186/1750-1172-2-47.
Zboralski, K. et al. (2008) ‘Quality of life and
emotional functioning in selected psychosomatic diseases’, Postepy Higieny i
Medycyny Doswiadczalnej, 62(February), pp. 36–41.












0 Comments